Call for Abstract
Scientific Program
9th World Congress on Breast Cancer & Therapy, will be organized around the theme “Global Burden of Breast Cancer - Prevention and Control ”
Global Breast Cancer Congress 2018 is comprised of 15 tracks and 86 sessions designed to offer comprehensive sessions that address current issues in Global Breast Cancer Congress 2018.
Submit your abstract to any of the mentioned tracks. All related abstracts are accepted.
Register now for the conference by choosing an appropriate package suitable to you.
Breast Cancer is the most common cause of death in women. We first need to understand how cancer develops in the body for reducing breast cancer risk. What is cancer and how it develops can help us find ways to slow down its progress or perhaps stop it from occurring in the first place. Current understanding of the biology of breast cancer is very important and its relevance to treating and preventing the disease. Breast cancer is not a one disease. For example, understanding that breast tissue of girls and young women is especially sensitive to cancer causing agents can help direct risk reduction efforts to these groups. Making sense of cancer denotes taking a step toward more apprised decisions about our bodies, ourselves and our environment.
Fig. Breast cancer showing an inverted nipple, lump, and skin dimpling
Source: https://en.wikipedia.org/wiki/Breast_cancer
Breast cancer knowledge and Characteristics gives the information of what is breast cancer, it helps to have some basic knowledge about the normal structure of the breasts and how it comes and what are the its characteristics. Breast Cancer develops through different stages. These stages may or may not eventually lead to metastatic and invasive cancer. In most cases it takes many years for cancer to develop. Early detection of any cancer is important because it increases the chances of removing the cancer before it becomes life-threatening. The Signs, symptoms and stages of Breast Cancer are also very important for curing the disease.
A risk factor is anything that affects your chance of getting a disease, such as cancer. But risk factors don't tell us everything. Having a risk factor, or even several, does not mean that you will get the disease. Most women who have one or more breast cancer risk factors never develop the disease, while many women with breast cancer have no apparent risk factors. The best weapon in the fight against breast cancer is the ability to stop the disease occurring in the first place. Breast cancer develops due to a combination of genetics, mutations, environmental and lifestyle factors. It is estimated that one in four breast cancers could be avoided by changing a range of lifestyle factors - for example, limiting alcohol intake, exercising more and maintaining a healthy bodyweight.
- Track 1-1Breast cancer knowledge and Characteristics
- Track 1-2Signs, symptoms and stages of Breast Cancer
- Track 1-3Breast Pathology and Breast Diseases
- Track 1-4Breast cancer host immune and stromal biology in cancer development
- Track 1-5Breast cancer Epidemiology and risk factors
- Track 1-6Environmental Factors
- Track 1-7Breast Cancer during Pregnancy
- Track 1-8Circulating Tumor Cells, Migration and Metastasis
- Track 1-9Line-1 Retransposan and Breast Cancer
- Track 1-10Breast Implants with Cancer-fighting and Healing Properties
- Track 1-11Monoclonal Antibodies
Survival is much higher when you pick up cancer in the early stages rather than the late stages. Performing screening is an effort to pick up breast cancer before there are any symptoms, so screening is the only for women who are not experiencing any kind of breast problems. The goal of screening exams for breast cancer is to identify cancers before they start to cause any symptoms. Early detection means using an approach or test that lets breast cancer get diagnosed earlier than otherwise might have occurred. Learning about Screening Tests and Diagnostic Tools for breast cancer is very important to kill the breast cancer in early stages. There are a number of ways to check for breast cancer. Some tests are basic; some are more invasive but provide more information. But all are vital to help detect this breast cancer disease in early.
Mammography is one of the most common screening test for breast cancer. A diagnostic mammogram is used to find breast disease in women who have breast symptoms or an abnormal result on a screening mammogram. Screening mammograms are used to look for breast disease in women who are asymptomatic; that is, those who appear to have no breast problems. The other types of screening and diagnostic tests are Biopsy, Sentinel node biopsy, Breast MRI and Breast Ultrasound.
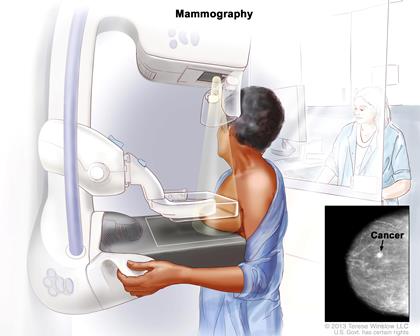
Fig: Mammography: The breast is pressed between two plates. X-rays are used to take pictures of breast tissue.
Source: https://www.cancer.gov/types/breast/patient/breast-treatment-pdq
The different breast cancer screening guidelines based on four distinct risk categories: women of moderate risk; women with at least one first-degree relative (i.e., parent or sibling) affected by breast cancer; women who have received a diagnosis of atypical hyperplasia (a form of benign breast disease) or lobular carcinoma in situ (cancers that are confined to the milk duct or lobule); and women with a history of mantle radiation (radiation received during treatment for Hodgkin disease).
- Track 2-1Biopsy and Sentinel node biopsy
- Track 2-2Mammography
- Track 2-3Ultrasound and MRI
- Track 2-4Blood and Genomic tests
- Track 2-5Diagnosis of Breast Cancer in Pregnant Womens
- Track 2-6An Update of Guidelines for Quality Assessment in Tumor Genetic Diagnostics
- Track 2-7Genetic counselling, pedigree based insight and personalized cancer management
Breast cancer can be divided into different types based on the way the cancer cells look under the microscope. Breast cancer can begin or start in different areas of the breast —the lobules, the ducts or in some cases, in between the tissue. In this section, you can learn about the different types of breast cancer, including invasive, non-invasive, recurrent, triple negative and metastatic breast cancers.
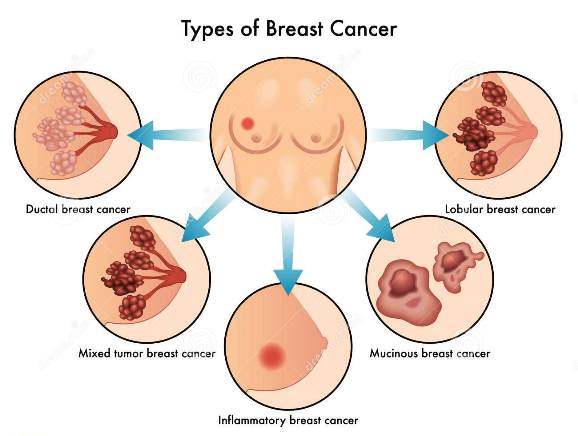
Inflammatory Breast Cancer (IBC) is a aggressive and rare form of breast cancer. According to the National Cancer Institute, about 1-5% of all breast cancer cases are inflammatory breast cancers in the United States. Inflammatory breast cancer usually starts with the reddening and swelling of the breast instead of a certain lumps. IBC tends to grow and spread quickly, with symptoms worsening within days or even hours. It’s important to recognize symptoms and seek prompt treatment. Although inflammatory breast cancer is a provoking diagnosis, keep in mind that treatments today are better at controlling the disease than in previous days.
Male Breast Cancer is a very rare disease. Male breast cancer is less than 1% of all breast cancers occur in men. In 2014, about 2,360 men are expected to be diagnosed with the disease. For men, the lifetime risk of being diagnosed with breast cancer is about 1 in 1,000. You may be thinking: Men don't have breasts, so how can they get breast cancer? The truth is that boys and girls, men and women all have breast tissue. The various hormones in girls' and women's bodies stimulate the breast tissue to grow into full breasts. Boys' and men's bodies normally don't make much of the breast-stimulating hormones. As a result, their breast tissue usually stays flat and small. Still, you may have seen boys and men with medium-sized or big breasts.
Invasive lobular Carcinoma (ILC) or infiltrating lobular carcinoma, is the second most common type of breast cancer after invasive ductal carcinoma (cancer that begins in the milk-carrying ducts and spreads beyond it). About 10% of all invasive breast cancers are invasive lobular carcinomas and it’s about 80% are invasive ductal carcinomas. Invasive means that the cancer has “invaded” or spread to the surrounding breast tissues. Lobular means that the cancer began in the milk-producing lobules, which empty out into the ducts that carry milk to the nipple. Carcinoma refers to any cancer that begins in the skin or other tissues that cover internal organs — such as breast tissue. All together, “invasive lobular carcinoma” refers to cancer that has broken through the wall of the lobule and start to invade the tissues of the breast. Over time, invasive lobular carcinoma can spread to the lymph nodes and possibly to spread to other areas of the body.
Paget disease of the nipple is one rare type of breast cancer starts in the breast ducts and spreads to the skin of the nipple and then to the areola, the dark circle around the nipple. It is rare and accounting for only about 1% of all cases of breast cancer. The skin of the nipple and areola often appears scaly, crusted, and red, with areas of bleeding or oozing. The woman may notice burning or itching. Phyllodes tumor is very rare breast tumor develops in the stroma or connective tissue of the breast, in contrast to carcinomas, which grows in the ducts or lobules. The other names for these tumors include cystosarcoma phyllodes and phylloides tumor. These tumors are usually benign but on rare occasions may be malignant. Benign phyllodes tumors are treated by removing the tumor along with a margin of normal breast tissue. A malignant phyllodes tumor is treated by removing it along with a wider margin of normal tissue, or by mastectomy.
- Track 3-1Ductal Carcinoma in Situ & Lobular Carcinoma in situ
- Track 3-2luminal A and B Breast cancer
- Track 3-3Inflammatory Breast Cancer
- Track 3-4Triple-Negative Breast Cancer
- Track 3-5Paget Disease of the Nipple and Phyllodes Tumor
- Track 3-6Metastatic Breast Cancer
- Track 3-7Male Breast Cancer
Estrogen therapy (ET) increases the estrogen level in your body. Estrogen impacts multiple systems of the body. Estrogen therapy (ET) is used to increase estrogen levels in postmenopausal women who have no uterus. This treatment may help prevent perimenopausal symptoms, osteoporosis, and colon cancer. Women in their 20s, 30s, and 40s who experience early menopause after having their ovaries removed (oophorectomy) or because of other medical reasons typically take ET to reduce their risk of early bone loss and osteoporosis. Historically, women have continued using ET for years beyond menopause. Women with a uterus who take estrogen also need the hormone progestin to prevent the estrogen from overgrowing the uterine lining, which can lead to endometrial (uterine) cancer. Estrogen-progestin is called hormone therapy (HT).
Breast Reconstruction:- Many women who have a mastectomy—surgery to remove an entire breast to treat or prevent breast cancer—have the option of having more surgery to rebuild the shape of the removed breast. Breast reconstruction surgery can be either immediate or delayed. With immediate reconstruction, a surgeon performs the first stage to rebuild the breast during the same operation as the mastectomy. A method called skin-sparing mastectomy may be used to save enough breast skin to cover the reconstruction. Breasts can be rebuilt using implants (saline or silicone) or autologous tissue (that is, tissue from elsewhere in the body). Most breast reconstructions performed today are immediate reconstructions with implants.
- Track 4-1Early & Advanced Breast Cancer Systemic Therapy
- Track 4-2Hormone Therapy and Combined Hormone Therapy
- Track 4-3Estrogen Replacement Therapy or Estrogen Therapy
- Track 4-4Biological Therapy (Herceptin)
- Track 4-5Breast Reconstruction Therapy
- Track 4-6Treatment of Breast Cancer During Pregnancy
Chemotherapy treatment uses medicine to weaken and destroy cancer cells in the body, including cells at the original cancer site and any cancer cells that may have spread to another part of the body. There are quite a few chemotherapy medicines. In many cases, a combination of two or more medicines will be used as chemotherapy treatment for breast cancer. Chemotherapy is used to treat early-stage invasive breast cancer to get rid of any cancer cells that may be left behind after surgery and to reduce the risk of the cancer coming back; advanced-stage breast cancer to destroy or damage the cancer cells as much as possible. Chemotherapy medicines prevent cancer cells from growing and spreading by destroying the cells or stopping them from dividing.
Adjuvant Therapy for breast cancer is any treatment given after primary therapy to increase the chance of long-term disease-free survival. Primary therapy is the main treatment used to reduce or eliminate the cancer. Not all women with breast cancer need adjuvant therapy. Patients at higher risk of cancer recurrence are more likely to need adjuvant therapy. Doctors look at both prognostic and predictive factors to decide which patients might benefit from adjuvant treatments. Prognostic factors help doctors estimate how likely a tumor is to recur. Predictive factors help doctors estimate how likely cancer cells are to respond to a particular treatment. Even in early-stage breast cancer, cells may break away from the primary tumor and spread to other parts of the body (metastasize). Therefore, doctors give adjuvant therapy to kill any cancer cells that may have spread, even if they cannot be detected by imaging or laboratory tests. Studies have shown that adjuvant therapy for breast cancer may increase the chance of long-term survival by preventing a recurrence.
Neoadjuvant Therapy is treatment given before primary therapy. A woman may receive neoadjuvant chemotherapy for breast cancer to shrink a tumor that is inoperable in its current state, so it can be surgically removed. A woman whose tumor can be removed by mastectomy may instead receive neoadjuvant therapy to shrink the tumor enough to allow breast-conserving surgery. Neoadjuvant chemotherapy is given in the same manner as adjuvant chemotherapy. If a tumor does not respond (shrink) or continues to grow during neoadjuvant chemotherapy, the doctor may stop treatment and try another type of chemotherapy or perform surgery instead, depending on the stage of the cancer. Clinical trials are examining whether hormonal therapy or trastuzumab is effective when given before surgery.
- Track 5-1Neoadjuvant Chemotherapy
- Track 5-2Adjuvant Chemotherapy
- Track 5-3Dose-dense Chemotherapy
- Track 5-4Combinational Chemotherapy
- Track 5-5Breast Cancer in Young Women and in Pregnancy
- Track 5-6 HER-2 Positive Breast Cancer
- Track 5-7Breast cancer, Psychosis and Schizophrenia
Many women who have a mastectomy—Surgery to remove an entire breast to treat or prevent breast cancer—have the option of having more surgery to rebuild the shape of the removed breast. Breast reconstruction surgery can be either immediate or delayed. With immediate reconstruction, a surgeon performs the first stage to rebuild the breast during the same operation as the mastectomy. A method called skin-sparing mastectomy may be used to save enough breast skin to cover the reconstruction. Breasts can be rebuilt using implants (saline or silicone) or autologous tissue (that is, tissue from elsewhere in the body). Most breast reconstructions performed today are immediate reconstructions with implants.
- Track 6-1Breast Reconstruction after Double Mastectomy
- Track 6-2 Breast Reconstruction Surgery Recovery
- Track 6-3Breast Reconstruction Images
- Track 6-4Breast Reconstruction Cost
- Track 6-5Breast Reconstruction after Radiation
Although breast cancer has historically been considered immunologically silent, several preclinical and clinical studies suggest that immunotherapy has the potential to improve clinical outcomes for patients with breast cancer. Overall, immunotherapy holds several key advantages over conventional chemotherapeutic and targeted treatments directed at the tumor itself. The common types of immunotherapy include Monoclonal antibodies, Cancer vaccines and Non-specific immunotherapies. One common type of breast cancer immunotherapy drug for breast cancer is Herceptin. This drug binds with specific proteins on breast cancer cells to slow or stop their growth. Your care team may recommend Herceptin to target breast tumors that produce too much of (or overexpress) a protein called HER2, which can also signal more aggressive cancers. Immunotherapy is a promising treatment for breast cancer, including advanced and recurrent forms of the disease. Immunotherapy may be used alone or in conjunction with other breast cancer treatments, such as radiation therapy and chemotherapy.
Radiation Therapy is treatment with high-energy rays or particles that destroy cancer cells. Radiation to the breast is often given after breast-conserving surgery to help lower the chance that the cancer will come back in the breast or nearby lymph nodes. Radiation may also be recommended after mastectomy in patients either with a cancer larger than 5 cm, or when cancer is found in the lymph nodes. Radiation therapy uses a special kind of high-energy beam to damage cancer cells. (Other types of energy beams include light and X-rays.) These high-energy beams, which are invisible to the human eye, damage a cell’s DNA, the material that cells use to divide. Radiation is an important and often necessary form of anti-cancer therapy because it is able to reduce the risk of recurrence after surgery. Many patients are surprised to discover that having radiation therapy is less difficult than they expected, though the radiation used to damage cancer in your body can also damage healthy cells.
How Radiation Works?? Radiation therapy uses a special kind of high-energy beam to damage cancer cells. (Other types of energy beams include light and X-rays.) These high-energy beams, which are invisible to the human eye, damage a cell’s DNA, the material that cells use to divide. Over time, the radiation damages cells that are in the path of its beam — normal cells as well as cancer cells. But radiation affects cancer cells more than normal cells. Cancer cells are very busy growing and multiplying — 2 activities that can be slowed or stopped by radiation damage. And because cancer cells are less organized than healthy cells, it's harder for them to repair the damage done by radiation. So cancer cells are more easily destroyed by radiation, while healthy, normal cells are better able to repair themselves and survive the treatment.
When Is Radiation Appropriate?? Radiation therapy has an important role in treating all stages of breast cancer because it is so effective and relatively safe. It may be appropriate for people with stage 0 through stage III breast cancer after lumpectomy or mastectomy. Radiation can also be very helpful to people with stage IV cancer that has spread to other parts of the body. Women who are pregnant should not have radiation. Radiation is never safe during pregnancy.
Types of Radiation Therapy:- There are three main types of radiation which are External Radiation, Internal Radiation and Intraoperative Radiation. External radiation is the most common type of radiation, typically given after lumpectomy and sometimes, mastectomy. In this section, you can read about how external radiation is given. Internal radiation is a less common method of giving radiation. It is being studied for use after lumpectomy. In this section, you can read about how radiation is delivered inside the breast. Another relatively new type of radiation to treat breast cancer is intraoperative radiation therapy (IORT). IORT is given during lumpectomy surgery after the cancer has been removed. In this section you can read about how intraoperative radiation therapy is given.
- Track 7-1Non Specific Immunotherapies
- Track 7-2 Immunotheraputic Approaches to Breast Cancer
- Track 7-3Immune Checkpoints & Cancer Therapy
- Track 7-4How Radiation Works & When is Radiation Appropriate ?
- Track 7-5 Types of Radiation Therapy, Radiotherapy New Techniques and Protocol
- Track 7-6Controversies in Radiation Therapy
- Track 7-7Monoclonal Antibodies
- Track 7-8Cancer Vaccines
Targeted Therapies is one of the innovative in breast cancer treatment. Several clinical trials led by physician-scientists at Mass General are revealing the power of new targeted anticancer therapies in breast cancer. Everolimus is a targeted therapy that works by zeroing in on the mTOR protein, which is regulated by the family of enzymes known as PI3 kinases (PI3K). In healthy cells, mTOR is involved in cell growth, cell proliferation, protein synthesis, and many other functions. In tumor cells, the mTOR pathway goes awry, leading to excess proliferation and a failure to respond to normal growth regulatory mechanisms. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer.
Surgery for Breast Cancer is really challenging to cure the breast cancer without any side effects. Lumpectomy is Surgery to remove the tumor along with some surrounding healthy tissue, leaving the margins (tissue bordering the tumor) free from cancer. Quadrantectomy is a breast-conserving surgery, this procedure removes one-fourth of the breast tissue. Mastectomy is a surgery to remove all the breast tissue. The most common type of mastectomy today is called a modified radical mastectomy, in which the breast tissue is removed but the muscles in the chest wall are spared, preserving arm strength. Lymphadenectomy is a surgery to remove one or more lymph nodes in the tumor area. Nodes are then examined for cancer by our pathology department. Oophorectomy is a removing the female ovaries to decrease hormone production. Plastic and Reconstructive Surgery are the surgeries to restore or improve the appearance of the breast. Some women choose to have reconstruction surgery at the time of a mastectomy; others defer a decision about reconstruction until a later time.
- Track 8-1 New trends to find breast cancer early
- Track 8-2Determining the best ways for hormonal therapy
- Track 8-3Anti- angiogenesis, Genetic risk and genetic testing (BRCA etc)
- Track 8-4Finding new Reconstructive Surgery Approaches
- Track 8-5Management of DCIS and ADH
- Track 8-6Molecular Cancer Therapeutics
- Track 8-7Targeted Therapies
- Track 8-8Surgery for Breast Cancer
- Track 8-9Developing ways to evaluate the Genes and Proteins in various Breast Cancer
Some breast cancer treatments can cause temporary side effects that stop soon after treatment finishes. However, your treatment may also cause short or longer-term side effects. Chemotherapy and radiation for breast cancer destroy constantly dividing breast cancer cells. But these treatments can also affect healthy cells. Medications and other self-help methods can help ease many of these side effects: Loss of appetite, Nausea and vomiting, Weakness and fatigue, Mouth soreness, Hair loss, Weight gain, Premature menopause, Lowered resistance to infections, Bleeding and Diarrhea. This section looks at some of the physical and emotional effects of breast cancer and its treatments and gives practical information about coping with them.
Sexuality and Intimacy is the major side effect in breast cancer women. Many women find sex and intimacy difficult after a breast cancer diagnosis. A serious illness in either partner can disrupt a sexual and intimate relationship, but breast cancer can cause unique problems. For example, some treatments can cause pain and sensitivity, while others can lead to menopausal symptoms, such as vaginal dryness. You may feel your body has betrayed you. And, after months of treatment, you may feel detached or disconnected from the pleasure your body once gave you. Body image issues may also affect how you view sex, as well as your sexuality. Exercise has been shown to help improve sexuality and body image concerns among breast cancer survivors. And, some research findings suggest that cognitive behavioral therapy (a special type of mental health counseling that may also combine techniques such as relaxation exercises) may improve sexual functioning for breast cancer survivors.
Lymphedema is a potential side effect of breast cancer surgery and radiation therapy that can appear in some people during the months or even years after treatment ends. Lymph is a thin, clear fluid that circulates throughout the body to remove wastes, bacteria, and other substances from tissues. Edema is the buildup of excess fluid. So lymphedema occurs when too much lymph collects in any area of the body. If lymphedema develops in people who’ve been treated for breast cancer, it usually occurs in the arm and hand, but sometimes it affects the breast, underarm, chest, trunk, and/or back. Why does lymphedema happen? As part of their surgery, many people with breast cancer have at least two or three lymph nodes removed from under the arm (sentinel lymph node biopsy), and sometimes many more nodes (axillary lymph node dissection). If the cancer has spread, it has most likely moved into to those underarm lymph nodes first because they drain lymph from the breast. Many people also need radiation therapy to the chest area and/or underarm. Surgery and radiation can cut off or damage some of the nodes and vessels through which lymph moves. Although there’s no way to know for sure whether you’ll develop lymphedema after breast cancer, you can help yourself by learning more about it. Know your risk factors, take steps to reduce your risk, and be aware of early symptoms. Left untreated, lymphedema can worsen and cause severe swelling and permanent changes to the tissues under the skin, such as thickening and scarring. With care, lymphedema can often be avoided or, if it develops, kept under control. Injury or infection involving the affected arm or hand can contribute to the development of lymphedema or make existing lymphedema worse, so preventive measures should focus on protecting the arm and hand.
- Track 9-1 Lymphedema after Breast Cancer Therapy
- Track 9-2 Breast Cancer treatment and Menopausal Symptoms
- Track 9-3 Lifestyle Changes after Treatment
Pathology is a medical specialty that underpins decision-making in many crucial steps of cancer care. Pathologists in many countries are medical doctors who are responsible for a wide – and rapidly growing – range of diagnostic reports on tissue that supports detection and characterization of disease, and informs the treatment and care carried out by surgeons, oncologists, radiotherapists and other health professionals in the cancer team.
Pathologists play a vital role in managing all types of cancer but their work can be compromised by lack of resources, training and multidisciplinary teamwork in hospitals, and a lack of commitment to a patient-center, accountable service at national level. They are often the ‘invisible’ members of the oncology team and should be available to meet patients and explain reports.
This manifesto sets out optimal requirements for a pathology service for breast cancer, but the principles are applicable to oncology generally. It is a call for all involved – pathologists, oncologists, patients, advocates, healthcare administrators and policymakers – to check and improve where necessary this vital discipline.
- Track 10-1Individuals – Professional Expertise and Development Requirements
- Track 10-2Departmental Requirements
- Track 10-3 Hospital Requirements
- Track 10-4Health System Requirements
- Track 10-5Breast Cancer Care Discussions
Phase 1 (phase I) trials study whether a new treatment is safe to use over a range of doses. The treatment may be given to people with different types of cancers.
A phase 1 trial is mainly a drug safety study.
Phase 2 (phase II) trials study how well a treatment works for a certain cancer, such as breast cancer. These trials may include between 25 and 100 people.
After a drug (or other therapy) is found to be effective in treating breast cancer in a phase 2 trials, a phase 3 trial will study it further.
Phase 3 (phase III) trials study how well a new treatment (including surgical procedures) works compared to the standard treatment (standard of care).
Phase 4 (phase IV) trials study the long-term side effects of treatments or answer new questions about the treatment.
- Track 11-1Phases of Trails
- Track 11-2Cohort and Case Studies
- Track 11-3Randomization
- Track 11-4 Screening and Prevention trials
- Track 11-5Pilot Studies and Feasibility Studies
During pregnancy your breasts change in readiness for breast feeding. The breast tissue becomes denser. This can make it more difficult to find changes in the breast that are due to cancer. The most common symptom of breast cancer is a lump. If you have a change that doesn’t go away after 2 to 4 weeks tell your doctor or midwife. Research shows that during pregnancy there is often a delay in diagnosis after women start to get breast symptoms. This is partly because breast cancer in pregnancy is so rare. It is also because the cancer can be difficult to diagnose because of the changes in the breast tissue. If the biopsy shows that you have cancer you may then have other tests to check the size of your cancer. Deciding which treatment to have and what that will mean for you and your developing baby can be very difficult. Doctors advise that your treatment should be as close as possible to what someone who isn’t pregnant would have. And whenever possible the treatment should not be delayed.
- Track 12-1Breast Cancer Treatment during Pregnancy
- Track 12-2Side Effects
- Track 12-3 Medication
Men have a little measure of nonfunctioning breast tissue (breast tissue that can't deliver drain) that is amassed in the range specifically behind the areola on the mid-section divider. Like breast tumor in ladies, disease of the male breast is the uncontrolled development with the potential for spread of a portion of the cells of this breast tissue. These phones turn out to be so anomalous in appearance and conduct that they are then called tumor cells. Breast tissue in both young men and young ladies comprises of tubular structures known as pipes. At pubescence, a young lady's ovaries create female hormones (estrogen) that cause the conduits to develop and drain organs (lobules) to create at the closures of the pipes. The measure of fat and connective tissue in the breast additionally increments as young ladies experience adolescence
- Track 13-1Symptoms of Breast Cancer in Men
- Track 13-2Risk factors for Breast Cancer in Men
- Track 13-3 Familial Predisposition
- Track 13-4Staging and Diagnosis
Breast cancer changes your life in different ways. Your body has changed suddenly because of surgeries, radiation given, and or chemotherapy treatments. All of these changes can imply your physical, social, and psychological status. Breast cancer rehabilitation is preferred for those who undergone lumpectomy with sentinel node biopsy treatment, lumpectomy with axillary dissection surgery, mastectomy, or breast reconstructive therapy, radiation and systemic chemotherapy. Chemotherapy and radiation and are dealing with the after effects of treatments, scar formation or radiation induced skin damages, mental and neural deficits such as memory or difficulty with executive planning. Rehabilitation therapists design personalized treatment plans to get back the patient to the highest level of normal functioning based on comprehensive assessment. Therapists do a comprehensive evaluation of each patient monitoring on functional abilities at present. Physicians design a program of therapeutic exercise and help you with progressing toward your functional attires. Rehabilitation and exercise program benefits includes improved strength in upper and lower body, greater flexibility in the shoulder joints and better body image.
- Track 14-1Physical Therapy
- Track 14-2Occupational Therapy
- Track 14-3Lymphedema Prevention and Treatment
- Track 14-4 Personalized Treatment Approach
- Track 14-5Auriculotherapy
- Track 14-6 Integrated Care
Breast Cancer therapeutic & market analysis assesses marketed and investigational products and combination regimens for the global breast cancer therapeutics market. Segmentation by drug class is provided, along with supporting information, such as clinical trial timelines and results, historical and projected launch timelines, and epidemiology. Marketed and pipeline products are broadly segmented into hormonal therapy, targeted therapy, chemotherapy, and other therapies of current global interest.

